Mohamad El Moheb, Mohammed Ghazi Sghaireen¹, Kiran Kumar Ganji², Kumar C Srivastava³, Deepti Shrivastava²
Private Practitioner, Les Pavillons Sous Bois, France, Departments of ¹Prosthodontics, ²Preventive Dentistry and ³Oral Medicine and Radiology, Oral and Maxillofacial Surgery and Diagnostic Sciences, College of Dentistry, Jouf University, Sakaka, Aljouf, Saudi Arabia
Abstract
The mucosal epithelium of the oral cavity plays a vital role in protecting the hard tissue, from mechanical, bacterial and chemical aggressions. This seal is made by the junctional epithelium and by collagen fibres. The screw bone builder (GF0) from TRATE, is a cover screw that will be used during the implant placement to cover the implant. The cover screw platform will not be in contact with the implant platform. After screwing the GF0, it will always maintain a space of 1mm between the two platforms implant and abutment. This space will be a room for the bone to grow and to fill this space. Hence this case series describes a modified cover screw to enhance long term bone stability around two‑stage implants.
Keywords: Bone, cover screw, implants
Introduction
Based on the Branemark protocol, the implant placed should be closed by a cover screw and the gingiva should be sutured. The implant platform and the cover screw are directly in contact with the internal aspect of the soft tissue including the connective tissue. [1] This direct contact between the soft tissue and the implant platform or the cover screw, do not keep any room for the bone to grow [2] on the top of the implant platform. A modification is done on this cover screw, to allow the bone to grow on the top of the implant platform. Since the introduction of the osseointergration principles by Branemark, [3] the two stages of surgery derive from this dogma. The Branemark protocol is based on the stability of the implant during 3–6 months to get a complete integration of the implant in the hard tissue. [4] During this period of consolidation, the implant is buried under the soft tissue and in an endosseous position which is covered by covering screw. [5] The implant is placed at bone level position. During the healing period, during the second‑stage surgery and placement of the healing abutment, the bone level was found, either at the implant neck or at the platform, due to crestal bone loss. A cover screw is developed to change the behavior of the crestal bone around the implant platform. This cover screw developed by TRATE on root form implant is called GF0 or screw bone builder. This case series will discuss the trial of the modified screw with its outcome and the importance of the growing bone on the top of the implant platform.
Rationale for modification of the cover screw
The mucosal epithelium of the oral cavity plays an important role in protecting the hard tissue, from mechanical, bacterial, and chemical aggressions. The natural dentition or implant‑supported emerge in the oral cavity by passing this barrier and compromising the seal. The mucosal response is creating a seal around the teeth or the implants, to make it impermeable to these aggressions [6] This seal is made by the junctional epithelium and by collagen fibers. These fibers are oriented perpendicularly to the natural root and even penetrate in the cementum, while around the implants these fibers are oriented parallel to the implant surface [Figure 1]. [6,7] This orientation of the collagen fibers determines the quality of the seal and the defense against aggression. The parallel orientation of the collagen fibers around the implants offers a poor seal and a weak resistance against the biological, mechanical, and chemical aggressions. [6] The thickness and the vascularization of the mucosa plays a crucial role in the seal and in the protection of the hard tissue and surrounding the root or the implant. The vascularization supplies nutrients and all needed cells for defense and repatriation.
The orientation of collagen fibers is not the only difference between the epithelium surrounding a natural tooth and an implant. The periodontal tissue surrounding teeth derives blood supply from the periosteum, periodontal ligament, and from the connective tissue. While the periodontal surrounding the implant gets its blood supply mainly from connective tissue [8,9] [Figure 2] and from the periosteum.
Since thevascular supply to peri‑implant tissue is limited and the collagen fibers are attached to the bone and not the implant surface hence the use of the screw bone builder allows to increase the periosteum surface. Increase in periosteum helps in increasing the bone level around the implant, by allowing the bone to grow on the top of the implant platform. Thus increasing of the bone surface will enhance the vascularization of the periosteum and will allow more collagen attachment on the top of the implant.
Screw design
The screw bone builder GF0 from TRATE, is a cover screw that was be used during the implant placement to cover the implant. The cover screw platform will not be in contact with the implant platform. After screwing the GF0 there will be always a space of 1 mm between the two platforms, the implant, and the abutment. This space will be the room for the bone to grow and to fill the space. The implant should be placed 1 mm under the bone level. The screw will act as a space maintainer to keep the space and to keep the soft tissue far from the implant platform. Since the soft‑tissue migration is ten times faster the other periodontal cells, [10] stopping their migration will give the chance to other cells to migrate and to fill the maintained space.

Figure 1: Arrangement of fibres (a) and corresponding blood supply (b) in around tooth and implant

Figure 2: Blood supply derived from periosteum around peri‑implant surface area
Clinical procedure
A total of ten patients were enrolled for the use of the screw bone builder. Two stage surgical technic, described by Branemark [11] was implemented to place thirty implants in ten enrolled patients using beta‑tricalcium phosphate and hydroxyapatite bone graft. In two cases, Polytetrafluoroethylene (PTFE) membranes reinforced with titanium were used to cover the graft. The eight other cases a collagen membrane was used. For the suturing PTFE threads were used. Five implants were placed after vertical augmentation for more than 6 mm. During the implant placement, the implant was placed 1 mm under the bone level. Moreover, the GF0 placed on the top of the implant. Operated site was sutured using PTFE sutures. Three months later, when all implants were uncovered for the second‑stage surgery to take out the GF0 and to place the healing screw, the bone level was measured to check if the bone is covering the implant platform.
After 3 months, all implants were osseointegrated. After raising the gingival flap, the GF0 appears at the bone level. When the GF0 was removed, it was not possible to see the implant platform. It was covered by a bony like tissue as evaluated by Albrektsson criteria [12] for success of implants [Figure 3‑7]. Two implants placed with a 6mm vertical augmentation showed bone loss six months after the loading. But during the second stage surgery, the implants were entirely covered by bony like tissue up till the implant platform.
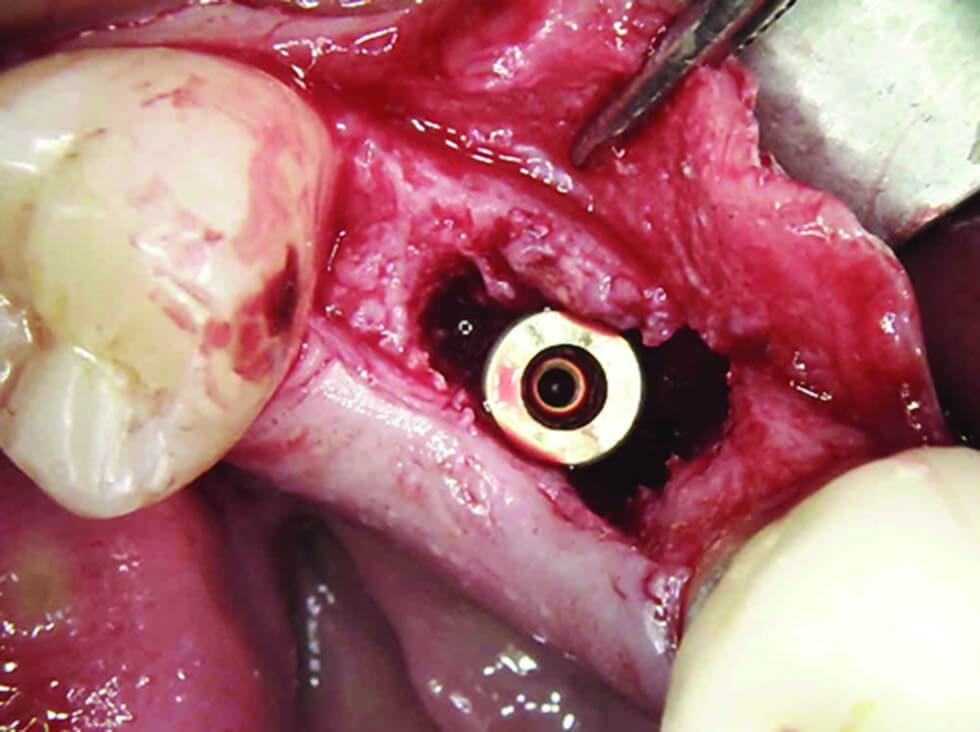
Figure 3: Implant placement subcrestal
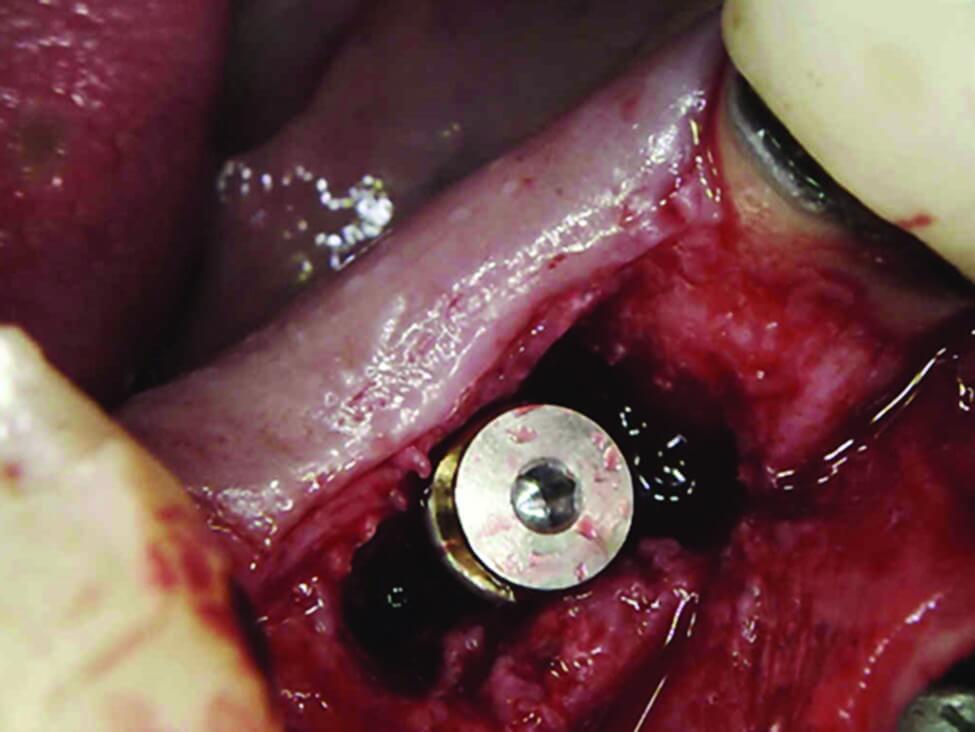
Figure 4: GF0 in place
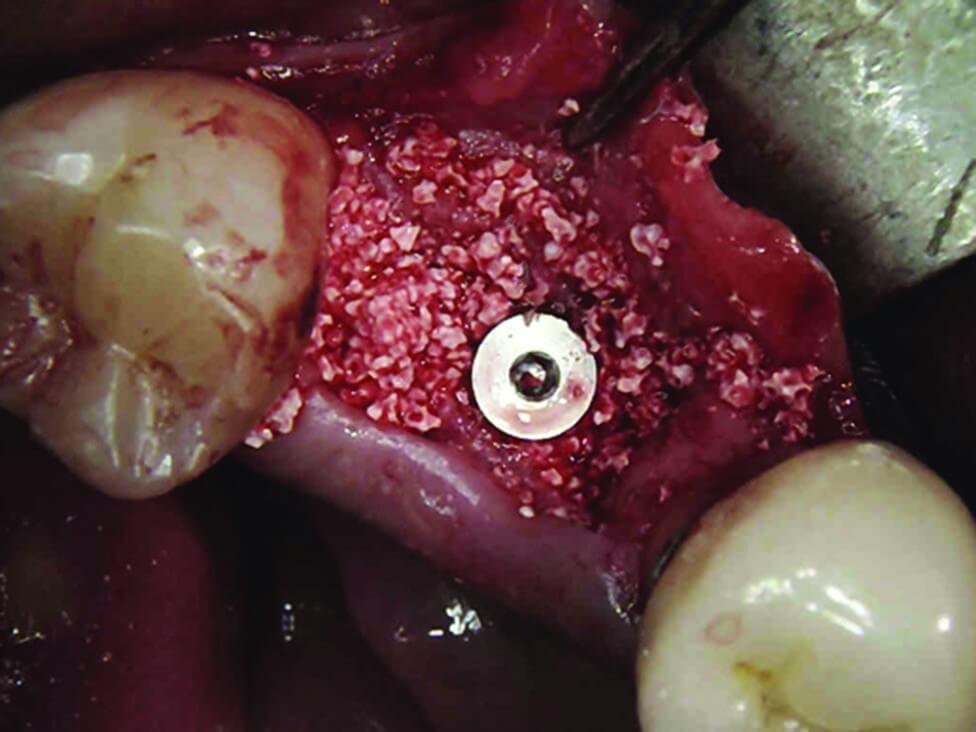
Figure 5: Bone grafting around the implant screw
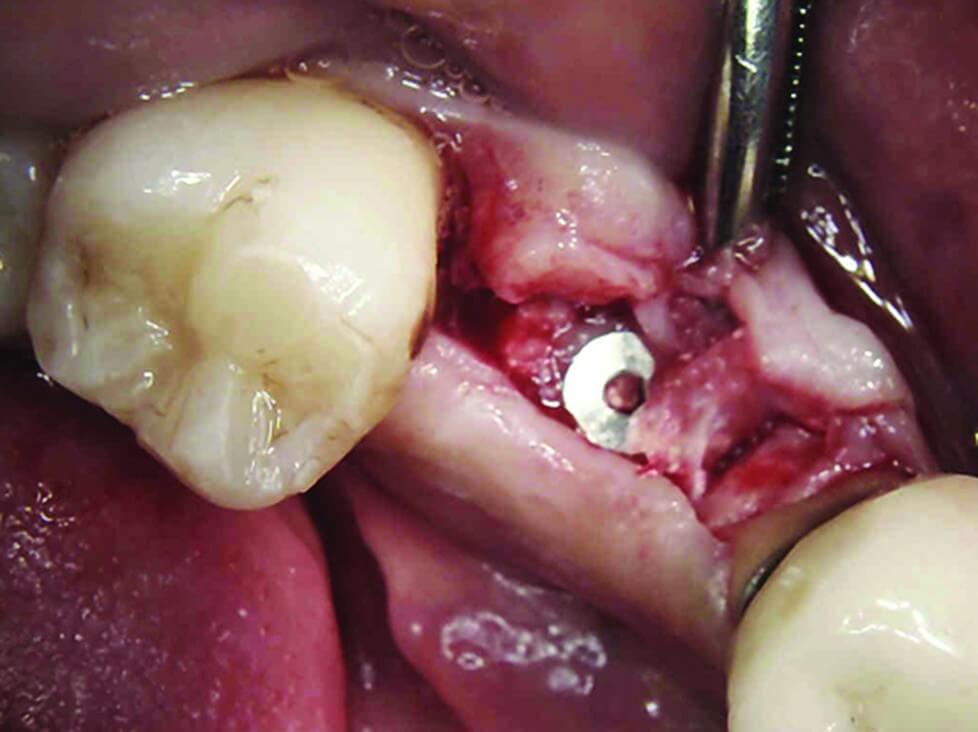
Figure 6: The GF0 after 3 months
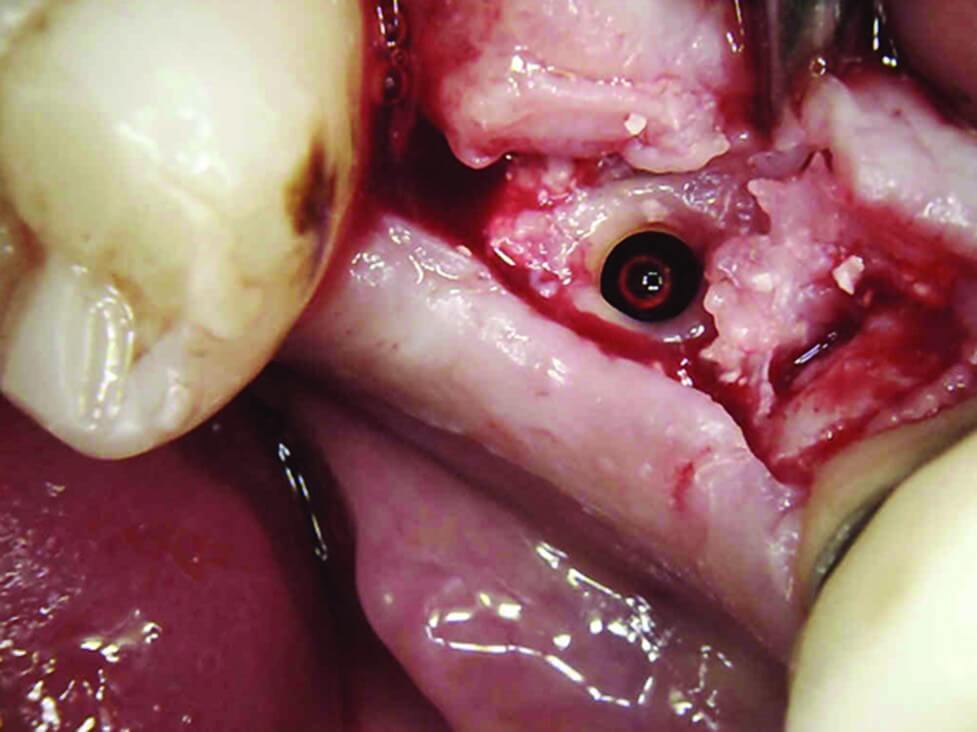
Figure 7: The bone is covering the implant platform
Discussion
The peri‑implant tissue status will condition the etiology of implant infection and bone loss. [13] The implant anatomy and the abutment‑implant connection type play an essential role in bone loss. [13,14] Having and maintaining reasonable and stable peri-implant mucosa is crucial in implant treatment. In addition to the patient hygiene and control, the surgeon should offer the best implant position with the maximum bone surrounding the implant and the highly vascularized soft tissue and with abundant collagen fibre attachment.
Recent report demonstrated that different microgap designs cause different shapes and sizes of the periimplant (‘dish shaped’) bone defects in submerged implants both in equicrestal and subcrestal positions. [15] Hence to prevent these bone defects, the implant should be in a position allowing the bone growth on the top of the implant neck. The aim of growing bone on the top of the implant platform is to maximize the periosteum around the implant and in this way maximizing the vascularization of the peri‑implant soft tissue, in the same way, this will offer more room to increase the collagen fiber attachment since the collagen will be attached to the bone and not to the implant surface nor the prosthetics. Increasing the bone will increase then the collagen attachment.
The implant placement under the bone level and the use of the GF0 will create a protected room and stopping the epithelium migration. This space will be filled with blood, and then a clot or a fibrin clot will fill this space. The bone cells will use this fibrin clot to migrate through this space and build a new bone. [16] To obtain the ideal conditions, the implant should be placed 1mm subcrustal. This subcrestal position of the implant requires the use of an appropriate implant. The implants with a morse or conical tapered connection can be placed in subcrestal without a significant loss of crestal and marginal bone. It even helps to maintain the bone level at the implant platform. [17] The subcrestal implant position shows less bone loss compared to equicrestal. [18] One of the major conditions for success in the subcrestal implant position is the implant‑abutment connection, that it should have less micro‑gap possible. [15] Therefore, conical connections are indicated to be used in this situation. [19, 20] The different roles insured by the GF0 maintains room during healing time for the bone cells to migrate and build bone on the above‑created space by this cover screw. The advantage of the GF0 allows the bone to obtain complete coverage of the implant platform by bone. This allows obtaining more extended periosteum, which means more vascular supply for the soft tissue and more closer collagen fibers attachment around the implant platform. Increasing the collagen fibers and collagen attachment will enhance the defense mechanism of this weak zone from where the peri‑implantitis starts. One of the major limitation of the proposed protocol would be uncontrolled bone growth over the GF0 hence it may require another surgery to remove and contour the bone overgrowth. Hermann and colleagues stated that the precise cause of the tissue changes was not known, but that one explanation was infection due to microgap leakage. [21] Recently proposed protocol to prevent marginal bone loss is Platform switch technique as introduced by Gardner and Lazzara and Porter. [22] Reports from a randomized clinical trial to evaluate the effect of Platform switch implants on peri-implant bone levels failed to confirm the hypothesis of reduced peri-implant bone loss for platform‑switched implants. [23‑25] The gap maintained would also provide a source for infection [26] if oral hygiene is not maintained properly there by strict oral hygiene aids are advisable in such circumstances.
Conclusion
The GF0 is a device developed to create and maintain a space over the implant platform. The GF0 will also keep the soft tissue far from the implant platform during the healing and the osseointegration period. These different roles insured by the GF0 keep the room all the healing time during to the bone cells to migrate and build bone on the above‑created space by this cover screw. The advantage of the GF0 allows the bone to obtain a complete coverage of the implant platform by bone. This will allow to get more extended periosteum which means more irrigation for the soft tissue and more and closer collagen fibers attached around the implant platform. Increasing the collagen fibers and collagen attach, will enhance the defense of this week zone, where the peri‑implantitis starts. With the limitation of this study, based on its clinical results, we can conclude that the GFO should be used each time and implant is placed on two stages or following Brandmark protocol.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Davarpanah M, Martinez H. Manuel D’implantologie Clinique. CDP; 2000. p. 117.
- Chasioti E, Chiang TF, Drew HJ. Maintaining space in localized ridge augmentation using guided bone regeneration with tenting screw technology. Q Int 2013;44:763-71.
- Brånemark PI, Hansson BO, Adell R, Breine U, Lindström J, Hallén O, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl 1977;16:1-132.
- Jokstad A. Osseointegration and dental implants: John Wiley & Sons; 2009.
- Misch CE. Contemporary Implant Dentistry-E-Book: Arabic Bilingual Edition: Elsevier Health Sciences; 2007.
- Atsuta I, Ayukawa Y, Kondo R, Oshiro W, Matsuura Y, Furuhashi A, et al. Soft tissue sealing around dental implants based on histological interpretation. J Prosthod Res 2016;3:1.
- Berglundh T, Lindhe J. Dimension of the periimplant mucosa. J Clin Periodontol. 1996;23:971-3.
- Bennani V, Schwass D. Nicholas chandler, gingival retraction techniques for implants versus teeth. JADA 2008;139:1354-63.
- Moon IS, Berglundh T, Abrahamsson I, Linder E, Lindhe J. The barrier between the keratinized mucosa and the dental implant. An experimental study in the dog. J Clin Periodontol 1999;26:658-63.
- Mali R, Priya Lele V. Guided tissue regeneration in communicating periodontal and endodontic lesions–A hope for the hopeless! J Indian Soc Periodontol 2011;15:410.
- Drage NA, Palmer RM, Blake G, Wilson R, Crane F, Fogelman I. A comparison of bone mineral density in the spine, hip and jaws of edentulous subjects. Clin Oral Implants Res. 2007;18:496-500.
- Albrektsson T, Zarb G, Worthington P, Eriksson A. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11-25.
- Jayachandran Prathapachandran NS. Management of peri-implantitis. Dent Res J (Isfahan). 2012;9:516.
- Caricasulo R, Malchiodi L, Ghensi P, Fantozzi G, Cucchi A. The influence of implant‐abutment connection to peri‐implant bone loss: A systematic review and meta‐analysis. Clin Implant Dent Relat Res. 2018;20:653-64.
- Weng D, Nagata MJH, Bell M, Bosco AF, De Melo LGN, Richter EJ. Influence of microgap location and configuration on the periimplant bone morphology in submerged implants. An experimental study in dogs. Clin Oral Implants Res. 2008;19:1141-7.
- Noori A, Ashrafi SJ, Vaez-Ghaemi R, Hatamian-Zaremi A, Webster TJ. A review of fibrin and fibrin composites for bone tissue engineering. International journal of nanomedicine. 2017;12:4937.
- Fetner M, Fetner A, Koutouzis T, Clozza E, Tovar N, Sarendranath A, et al. The Effects of Subcrestal Implant Placement on Crestal Bone Levels and Bone-to-Abutment Contact: A Microcomputed Tomographic and Histologic Study in Dogs. Int J Oral Maxillofac Implants. 2015;30.
- Valles C, Rodriguez-Ciurana X, Clementini M, Baglivo M, Paniagua B, Nart J. Influence of subcrestal implant placement compared with equicrestal position on the peri-implant hard and soft tissues around platform-switched implants: A systematic review and meta-analysis. Clin Oral Investig. 2018;22:555-70.
- Macedo JP, Pereira J, Vahey BR, Henriques B, Benfatti CA, Magini RS, et al. Morse taper dental implants and platform switching: The new paradigm in oral implantology. European journal of dentistry. 2016;10:148-54.
- Larrucea Verdugo C, Jaramillo Núñez G, Acevedo Avila A, Larrucea San Martín C. Microleakage of the prosthetic abutment/implant interface with internal and external connection: In vitro study. Clin Oral Implants Res. 2014;25:1078-83.
- Hermann JS, Schoolfield JD, Schenk RK, Buser D, Cochran DL. Influence of the size of the microgap on crestal bone changes around titanium implants. A histometric evaluation of unloaded non‐submerged implants in the canine mandible. J Periodontol. 2001;72:1372-83.
- Lazzara RJ, Porter SS. Platform switching: a new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent. 2006;26.
- Vigolo P, Givani A. Platform-switched restorations on wide-diameter implants: a 5-year clinical prospective study. Int J Oral Maxillofac Implants. 2009;24.
- Enkling N, Jöhren P, Klimberg V, Bayer S, Mericske‐Stern R, Jepsen S. Effect of platform switching on peri‐implant bone levels: a randomized clinical trial. Clin Oral Implants Res. 2011;22:1185-92.
- Hsu JT, Fuh LJ, Lin DJ, Shen YW, Huang HL. Bone strain and interfacial sliding analyses of platform switching and implant diameter on an immediately loaded implant: Experimental and three‐dimensional finite element analyses. J Periodontol. 2009;80:1125-32.
- Norton MR. Multiple single-tooth implant restorations in the posterior jaws: maintenance of marginal bone levels with reference to the implantabutment microgap. Int J Oral Maxillofac Implants. 2006;21.

